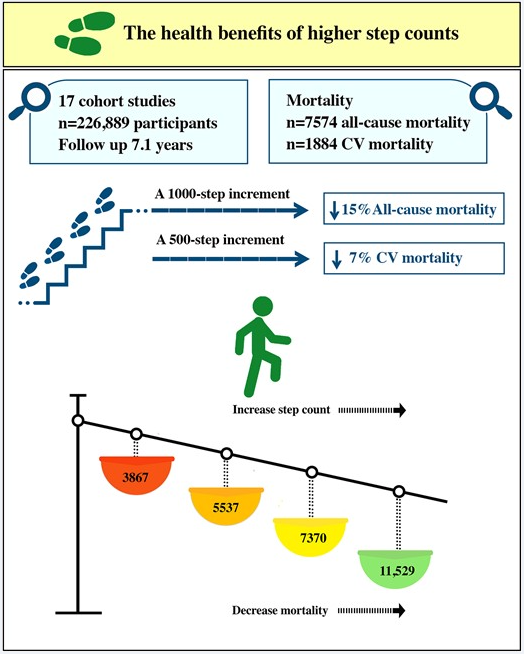
If you’ve been paying attention AT ALL, then you know we’ve talked about getting up and moving. We’ve previously debunked the “you gotta get 10,000 steps”, but at the same time, more is better. Here’s a tidy summary of lots of walking data over years that again supports the idea that doing more is better. Simply, if you add 1000 steps to your daily routine you can expect a 15% reduction on overall mortality (that’s a population risk – we usually only get to die once), while 500 steps will buy you a 7% reduction in cardiovascular risk.
I’m going to say it again – EXERCISE is the single most important thing you can do to improve your overall health, reduce your risk of chronic disease, and extend your life and healthspan. I am happy to assist you in developing a specific program to directly address your specific needs. Just give me a call and we can get started.
FROM THE EUROPEAN JOURNAL OF PREVENTIVE CARDIOLOGY / BY MACIEJ BANACH, JOANNA LEWEK, STANISŁAW SURMA, PETER E PENSON, AMIRHOSSEIN SAHEBKAR, SETH S MARTIN, GANI BAJRAKTARI, MICHAEL Y HENEIN, ŽELJKO REINER, AGATA BIELECKA-DĄBROWA, IBADETE BYTYÇI
The association between daily step count and all-cause and cardiovascular mortality: a meta-analysis
Lay Summary
There is strong evidence showing that sedentary life may significantly increase the risk of cardiovascular (CV) disease and shorten the lifespan. However, the optimal number of steps, both the cut-off points over which we can see health benefits, and the upper limit (if any), and their role in health are still unclear.
In this meta-analysis of 17 studies with almost 227 000 participants that assessed the health effects of physical activity expressed by walking measured in the number of steps, we showed that a 1000-step increment correlated with a significant reduction of all-cause mortality of 15%, and similarly, a 500-step increment correlated with a reduced risk of CV mortality of 7%. In addition, using the dose–response model, we observed a strong inverse nonlinear association between step count and all-cause mortality with significant differences between younger and older groups.
It is the first analysis that not only looked at age and sex but also regional differences based on the weather zones, and for the first time, it assesses the effect of up to 20 000 steps/day on outcomes (confirming the more the better), which was missed in previous analyses. The analysis also revealed that depending on the outcomes, we do not need so many steps to have health benefits starting with even 2500/4000 steps/day, which, in fact, undermines the hitherto definition of a sedentary life.
Abstract Aims
There is good evidence showing that inactivity and walking minimal steps/day increase the risk of cardiovascular (CV) disease and general ill-health. The optimal number of steps and their role in health is, however, still unclear. Therefore, in this meta-analysis, we aimed to evaluate the relationship between step count and all-cause mortality and CV mortality.
Methods and results
We systematically searched relevant electronic databases from inception until 12 June 2022. The main endpoints were all-cause mortality and CV mortality. An inverse-variance weighted random-effects model was used to calculate the number of steps/day and mortality. Seventeen cohort studies with a total of 226 889 participants (generally healthy or patients at CV risk) with a median follow-up 7.1 years were included in the meta-analysis. A 1000-step increment was associated with a 15% decreased risk of all-cause mortality [hazard ratio (HR) 0.85; 95% confidence interval (CI) 0.81–0.91; P < 0.001], while a 500-step increment was associated with a 7% decrease in CV mortality (HR 0.93; 95% CI 0.91–0.95; P < 0.001). Compared with the reference quartile with median steps/day 3967 (2500–6675), the Quartile 1 (Q1, median steps: 5537), Quartile 2 (Q2, median steps 7370), and Quartile 3 (Q3, median steps 11 529) were associated with lower risk for all-cause mortality (48, 55, and 67%, respectively; P < 0.05, for all). Similarly, compared with the lowest quartile of steps/day used as reference [median steps 2337, interquartile range 1596–4000), higher quartiles of steps/day (Q1 = 3982, Q2 = 6661, and Q3 = 10 413) were linearly associated with a reduced risk of CV mortality (16, 49, and 77%; P < 0.05, for all). Using a restricted cubic splines model, we observed a nonlinear dose–response association between step count and all-cause and CV mortality (Pnonlineraly < 0.001, for both) with a progressively lower risk of mortality with an increased step count.
Conclusion
This meta-analysis demonstrates a significant inverse association between daily step count and all-cause mortality and CV mortality with more the better over the cut-off point of 3967 steps/day for all-cause mortality and only 2337 steps for CV mortality.